The effectiveness of a blind blood patch at the L1-2 level for the treatment of spontaneous intracranial hypotension
Article information
Abstract
Objective
Spontaneous intracranial hypotension (SIH) is characterized by orthostatic headache due to cerebrospinal fluid (CSF) leakage with an unknown cause. The treatment of SIH includes conservative treatment, such as bed rest and fluid infusion, or surgical repair of the dural defect; however, in recent years, epidural blood patch (EBP) has emerged as a treatment of choice when conservative treatment is ineffective.
Methods
Between January 2015 to April 2021, we performed blind EBP in 17 patients who did not show any improvement in response to conservative treatment. The sites of CSF leakage were different in each patient, but all EBPs were performed at the L1–2 level.
Results
Of the 17 patients who received blind EBP, 10 (58.8%) showed immediate symptomatic relief and no recurrence. Seven patients (41.2%) failed to improve clinically after the first blind EBP, and all of those seven patients underwent repeated blind EBP at the same level. After the second EBP, all patients showed no residual symptoms and no recurrence.
Conclusion
Blind EBP is a safe and easy option for the treatment of SIH, and the L1–2 level deserves consideration as an effective location for performing blind EBP.
INTRODUCTION
Spontaneous intracranial hypotension (SIH) first described by Schaltenbrand is a syndrome in which a orthostatic headache occurs due to an unknown cause of cerebrospinal fluid (CSF) leakage, and may be accompanied by posterior neck pain, nausea, vomiting, dizziness, and changes in hearing and vision [1,2]. SIH is not uncommon with an annual incidence of 5 per 100,000 individuals per year and typically encountered in middle age and showed female preponderance [2,3].
Diagnostic exams including lumbar puncture, radioisotope cisternography, computed tomography myelography (CTM), and magnetic resonance myelography are performed for suspected patients. Although various neuroimaging features of SIH has been suggested, such diagnostic findings are not always noticed [4-6].
The treatment of SIH includes conservative treatments such as bed rest and fluid infusion or surgical repair of dural defect, but recently, when conservative treatment is ineffective, epidural blood patch (EBP) is a treatment of choice [3,7-9]. The mechanism of EBP has not been determined, but may involve a temporary increase in epidural pressure, the sealing of a tear by coagulating injected blood, or the initiation of inflammatory reactions that promote dural tear healing [8,10-12]. EBP is divided into a blind EBP, which is performed regardless of the location of CSF leakage, and a targeted EBP, which is performed to the location of CSF leakage [4]. There is debate which one is better [5,7,8,13,14].
We retrospectively reviewed our cases of SIH treated with blind EBP and compared the result with that of targeted EBP through wide literature review.
MATERIALS AND METHODS
Study population
This retrospective study reviewed the data on patients with orthostatic headache from a single center from January 2015 to April 2021 (76 months). The patients had undergone brain magnetic resonance imaging (MRI) with gadolinium enhancement and CTM. In total, 17 patients who had been diagnosed with SIH according to the International Classification of Headache Disorders criteria for headache were enrolled [15]. In most patients, brain MRI revealed contrast enhancement and thickening of pachymeninges, compatible with the typical radiologic findings of SIH. To confirm sites of CSF leakage accurately, we performed CTM. After diagnosis of SIH, patients were treated using conservative management for at least 1 week.
Epidural blood patch
All 17 patients were admitted to the neurology department and did not show any improvement with the conservative treatment, so blind EBPs were performed at the L1–2 level after transfer to the neurosurgery department. The entire procedure was executed with fluoroscopic guidance at the angio suite. EBPs were performed using a 21-gauge Tuohy needle via a midline interlaminar approach with the patient lying in a prone position. The epidural space was identified using the loss of resistance technique, and accurate localization was finally confirmed by epidurography under fluoroscopy.
After that, under fluoroscopic guidance, 15–22 mL of autologous blood mixed with contrast medium in a ratio of 2:1 (blood:contrast) was slowly injected. Then, follow-up fluoroscopic image confirmed the wide-spreading of autologous blood (Fig. 1). All patients underwent post-procedure spinal computed tomography (CT) instantly after EBP to confirm the widespread of patched blood (Fig. 2). In cases showing recurrence of orthostatic headache after EBP, we performed repeat EBP. Follow-up periods ranged from 12 months to 2 years with a mean of 16.1 months (Table 1).
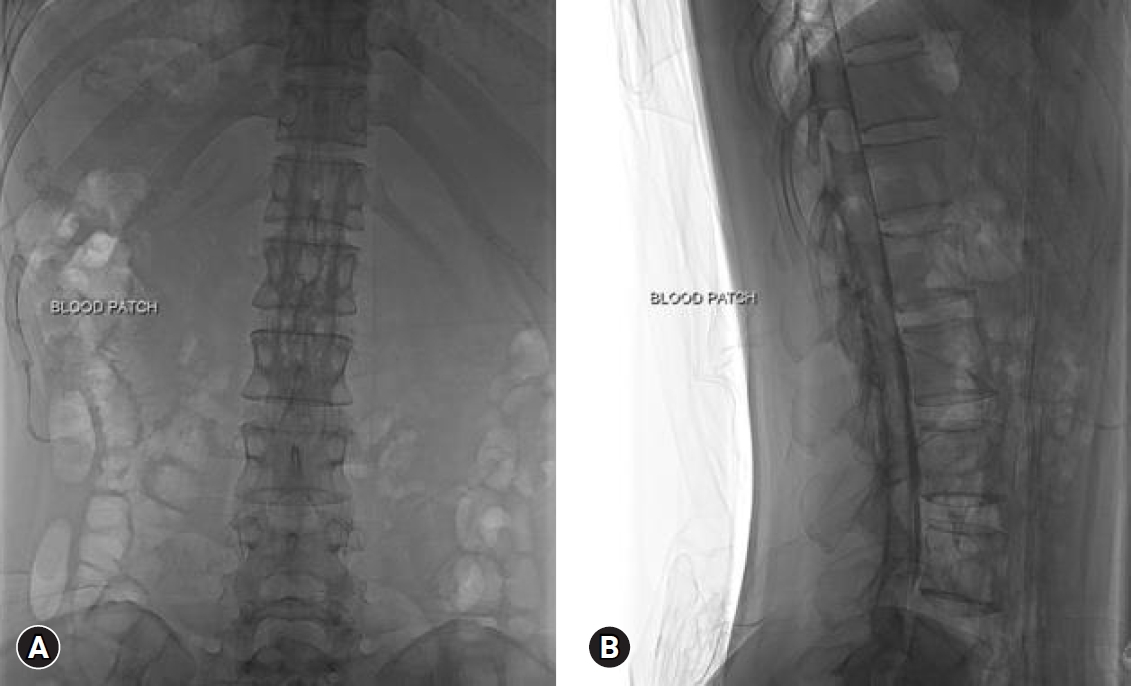
Blind epidural blood patch under intraoperative fluoroscopic guidance. Epidural puncture was performed at the L1–2 level. Widespread of a mixture of contrast medium and autologous blood was visualized over the thoracic and lumbar spine on the anteroposterior view (A) and lateral view (B).
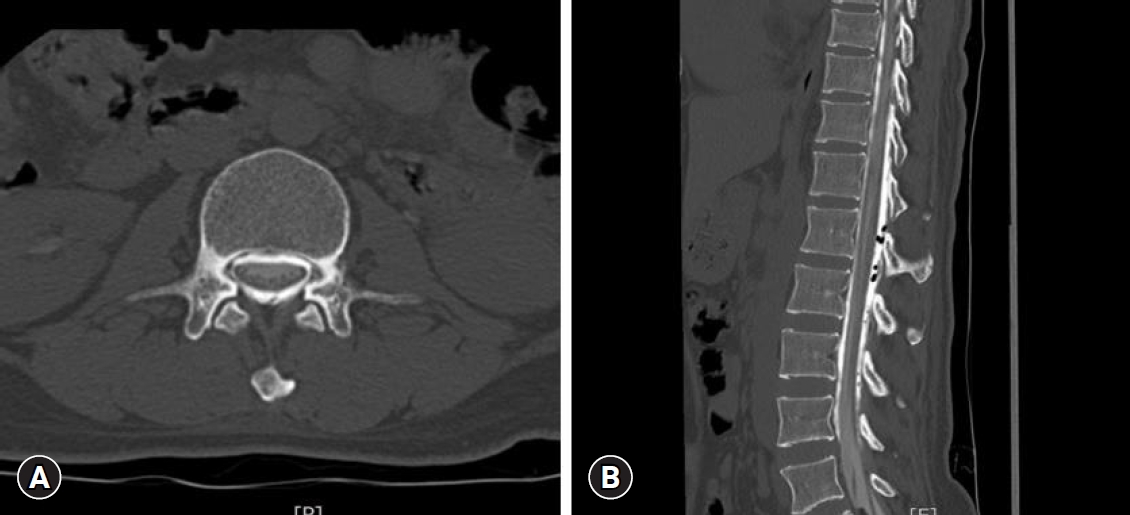
(A, B) Postoperative non-contrast computed tomography showing a hyperdense collection of patched blood along the epidural space.
Treatment outcomes
The effects of each treatment method were evaluated for degree and duration of symptom relief, and number of repeat EBPs. To evaluate treatment outcome, we defined a poor outcome as a persistent symptom or sign requiring repeat EBP, and a good outcome as complete recovery or minimal symptoms requiring only medication, such as nonsteroidal anti-inflammatory drugs, for mild symptom relief. We investigated the clinical courses of the 17 patients by reviewing medical records and follow-up data from our outpatient department.
Ethical statements
This study was approved by the Institutional Review Board of Chosun University Hospital (approval number: 2020-12-065). All the procedures were performed according to the ethical standards of the institutional and national research committees and the Declaration of Helsinki. The requirement for informed consent was waived due to the retrospective nature of the study.
RESULTS
All 17 patients (9 male and 8 female) that EBP performed for the treatment of SIH were identified. Mean age was 44 years old (range 20–69 years). All patients presented with severe orthostatic headache. In addition, 5 patients (29.4%) presented with nausea/vomiting and 4 patients (23.5%) presented with dizziness. The mean duration of symptoms was 12.2 days, and symptoms persisted about 2 weeks even in conservative therapy, such as hydration and bed rest. A localized leakage was identified in 14 patients (82.4%) by CTM. The locations of CSF leakage were as follows: cervico-thoracic, 1 patient; thoracic, 2 patients; thoraco-lumbar, 2 patients; lumbar, 9 patients; and unknown, 3 patients (Table 1). Brain CT and MRI were performed in all patients at the initial diagnosis. Diffuse pachymeningeal enhancement was the most common finding. Several patients presented downward displacement of the tonsil and obliteration of the prepontine cistern.
All patients underwent blind EBPs with fluoroscopic guidance. The EBP was performed at the L1–2 level regardless of the location of CSF leakage. The mean blood volume used for the first EBP was 18.5 mL (range 15–21 mL). The mean blood volume was higher in the good outcome group than the poor outcome group (20.1 mL vs. 16.2 mL). Of the 17 patients who received a blind EBP, 10 patients (58.8%) experienced immediate symptomatic relief and no recurrence and 7 patients (41.2%) failed to improve clinically after the first blind EBP (Table 1). All 7 patients failed to the first EBP underwent repeat blind EBPs at the L1–2 level. The mean amount of blood volume used for the second EBP was 21.2 mL (range 20–23 mL). After a second blind EBP, all 7 patients showed no recurrence or residual symptoms (Table 2).
DISCUSSION
SIH is first described by Schaltenbrand [1]. SIH is a syndrome of low CSF volume and pressure caused by persistent CSF leakage through a dural defect. This leads to downward migration of the brain, causing various symptoms. Orthostatic headache is the most common and cardinal clinical symptom. In the 50% of patients, other symptoms are accompanied by orthostatic headache; posterior neck pain, neck stiffness, nausea, vomiting, etc. [2]. Estimates suggest that the annual incidence of SIH is 5 per 100,000 individuals per year [3]. SIH is typically encountered in middle age (30–50 years of age) and has a predilection for female (female:male=2:1) [14]. The diagnosis of SIH is not simple. Schievink [2] reported 17 of 18 patients (94%) were misdiagnosed initially and the median diagnostic delay was 5 weeks despite invasive diagnostic procedures were done in some patients. For this reason, it is essential to carefully check the patient's history and check appropriate diagnostic test. According to the Monroe-Kelly hypothesis, as the intracranial CSF decreases, the intracranial blood volume increases to compensate for this. Due to this, diffuse pachymeningeal enhancement and enlargement and engorgement of pituitary gland appear, which can be confirmed by gadolinium-enhanced brain MRI. Watanabe et al. [4] reported on the diagnostic usefulness of MRI. However, since brain MRI showed no abnormal findings in about 19% of patients with SIH and can’t give information about the leakage sites, additional spinal imaging is required if active treatment is being considered [16]. There are no guidelines widely acknowledged for the treatment of SIH yet. According to meta-analysis about SIH, conservative treatment including bed rest, hydration, analgesia, steroids, caffeine was effective in about 24.5% of 881 patients for a period ranging from 7 to 9 weeks [7,17]. EBP is commonly used treatment to patients showed no response to conservative treatment. Autologous blood injection to epidural space, aka ‘epidural blood patch’, was first described by Gormley [16] in 1960. Even though EBP is commonly used for the treatment of SIH, the process how it acts has not been determined, but may involve a temporary increase in epidural pressure, the sealing of a tear by coagulating injected blood, or the initiation of inflammatory reactions that promote dural tear healing [8,10-12]. According to previous studies, the therapeutic effect of EBP showed various improvement rate in 64–93% of patients after first treatment [7,13,18-20]. There are two methods of EBP, targeted and non-targeted one. There is controversy over which EBP is more effective. Some authors reported the superiority of targeted EBP [8,14,21]. Cho et al. [8] reported the success rate after the first targeted EBP was 87.1%, as compared with 52% for non-targeted EBP. Targeted EBP may cause serious complications including compression of the spinal cord and nerve roots, chemical meningitis, intrathecal injection of autologous blood, and neck stiffness. Beside, due to the anatomy of the cervical or thoracic level, small amount of blood can be injected relatively as compared with the lumbar level [8]. Because of these risks, some authors prefer the blind EBP [22,23]. Ferrante et al. [24] reported 90% success rate of blind EBP. In our study, we performed blind EBPs on the L1–2 level according to the hypothesis presented by Franzini et al. [9]. Franzini et al. [9] proposed a hypothesis about the pathophysiologic mechanism of SIH between the CSF and the venous drainage of the spinal epidural space. Negative pressure within the inferior vena cava (IVC) will result in overdrainage of venous blood from the epidural spinal vein network via large lumbar collectors through 1-way valves. A decrease in spinal epidural pressure and volume of epidural veins result in modification of the epidural gradient between epidural space pressure (negative) and CSF pressure (positive in orthostatic conduction). This modification results in aspiration of CSF into the spinal space and veins. They proposed the technique aimed to provoke a marked rise in epidural pressure to reverse the CSF-hematic gradient, thus removing the main etiopathogenetic factor that is the epidural hypotension maintained by the epidural venous drainage through the IVC. The L1–2 level is the target for helping reversing the CSF-blood gradient within the epidural space along the entire cord, not for the sealing of leakage point.
We performed all blind EBPs at the L1–2 levels regardless of leakage points for the following reasons.
I. Following the hypothesis and techniques Franzini et al. [9] suggested. But, we didn’t use the fibrin glue because not to want to take the risk of complications due to the cord compression.
II. It is technically easier than performing EBP to the epidural space at the thoracic level.
III. As an intermediate point between the lumbar and thoracic region, the locational advantage of being easy to spread patched blood was considered. In fact, considering the postoperative fluoroscopic images that the contrast agents were widely spread in the thoracolumbar area and the symptom improvement rate was high in the cases of applying a high volume of blood, it would be difficult to rule out the possibility that it was not because of Franzini’s hypothesis, but because of the locational advantage.
Our series had a few significant limitations. We performed retrospective chart and image reviews. Therefore, we could not eliminate biases inherent of retrospective reviews. SIHs are not a common disease entity. Thus, we did not experience the sufficient cases to confirm the efficacy of blind EBP. Because the mean follow-up period in our series was short, there is the possibility that the recurrence rate was underestimated. Due to the small size of our study, we could not rule out the chance that the favorable results were somewhat exaggerated. The favorable results of our cases do not necessarily mean that blind EBP is the treatment of choice for SIHs. However, this technique is a safe and technically easy treatment option that physicians should consider when they encounter this disease entity.
CONCLUSION
Blind EBP is a safe, easy option for the treatment of SIH and the L1–2 level deserves consideration as an effective location for performing blind EBPs.
Notes
CONFLICTS OF INTEREST
No potential conflict of interest relevant to this article was reported.
Acknowledgements
We would like to thank all those who were involved in data collection.
This study was supported by research funding from Chosun University Hospital, 2020.


