 |
 |
| Neurofunction > Volume 17(2); 2021 > Article |
|
Abstract
In rare cases, head trauma can cause epidermal cell invasion into the intracranial space. A 72-year-old man visited our outpatient clinic with abnormal brain magnetic resonance imaging findings. The patient experienced head trauma 20 years ago and complained of progressive cortical impairment 1 year previously. Radiologic findings revealed an 8-cm lobulated tumor in the right occipital convexity with inner calcification and invasion in the dura mater and bone tissue, causing a mass effect. The tumor was assumed to be an atypical meningioma or bone mass. We planned craniectomy, tumor removal, and bone reconstruction. The intraoperative findings included a cystic capsulated tumor with dura mater and skull invasion. After capsule removal, we observed liquified tumor contents with keratin-like material. After surgery, the pathologic report confirmed that the tumor was an epidermoid cyst. On follow-up magnetic resonance imaging, there was no evidence of a remnant tumor. At an outpatient follow-up visit, it was confirmed that the patient had improved performance (modified Rankin scale=2), a mini mental state examination score of 17/30, and physical location awareness. In post-traumatic calcified epidermoid cysts, surgery can be helpful for recovering patientsŌĆÖ neurological deficits by decreasing the mass effect.
Intracranial epidermoid cysts (IECs) are uncommon, with an incidence of 0.1-0.8% of all intracranial tumors [1,2]. Most are typically observed as congenital diseases in children and are due to remaining ectodermal tissues from the disruption of neural tube closure [1]. Although acquired epidermoid cysts rarely occur, trauma can lead to implantation of epidermal cells in the intracranial space [3].
Herein, we present a case in which trauma led to a large epidermoid cyst in the posterior fossa, causing cortical dysfunction, and where surgical resection improved symptoms.
A 72-year-old man with a history of diabetes mellitus and hyperlipidemia visited the outpatient clinic of Department of Neurology to improve his gradual decrease in cortical function. He had a history of head trauma in a motorcycle accident 20 years ago with deep laceration of occipital area but suffered no hemorrhage at the time, and of penetrating trauma in the left eye and blindness 15 years ago.
The patient complained of a lack of time and place orientation and memory impairment, especially recent memory. Cortical impairment was confirmed with a modified Rankin scale (mRs) score of 3 and Korean mini mental state examination (K-MMSE) score of 16/30. He also showed incapacity for calculation and writing so was subjected to magnetic resonance imaging (MRI) for further evaluation.
On MRI (Fig. 1), an 8 cm multi-lobulated tumor with inner calcification was observed lining the right occipital convexity, around the site of the previous accident. It caused parenchymal compression due to mass effects. The heterogeneous mass with hypo-intensity at T1 and high-intensity at T2 showed direct dura mater invasion and destruction of bone structures.
The patient visited our outpatient clinic to determine whether surgical treatment was required. On computed tomography findings (Fig. 2), both a low-density fluid pattern and some soft tissue density were observed with calcification at the border. Perilesional swelling was not visible, and contrast not enhanced.
We speculated that the tumor was an atypical or malignant meningioma or an epidermoid cyst and planned surgical treatment. We used the previous laceration site as an incision site for craniectomy. After the right parieto-occipital craniectomy, destructed fragments of bone, muscles and fascia were observed. A mass in the form of an encapsulated cyst was observed with signs of invasion in the dura mater and bone. After opening the capsule membrane, the content appeared to be liquefied, and keratin-like substances were observed. After taking a frozen biopsy, nearly total tumor resection was achieved and a bone cement flap put in place.
Pathologic examination of the biopsy (Fig. 3) confirmed the mass to be an epidermoid cyst. It was lined with stratified squamous epithelium and accumulated epithelial cell fragments and keratin were observed. No other skin adnexa were visible.
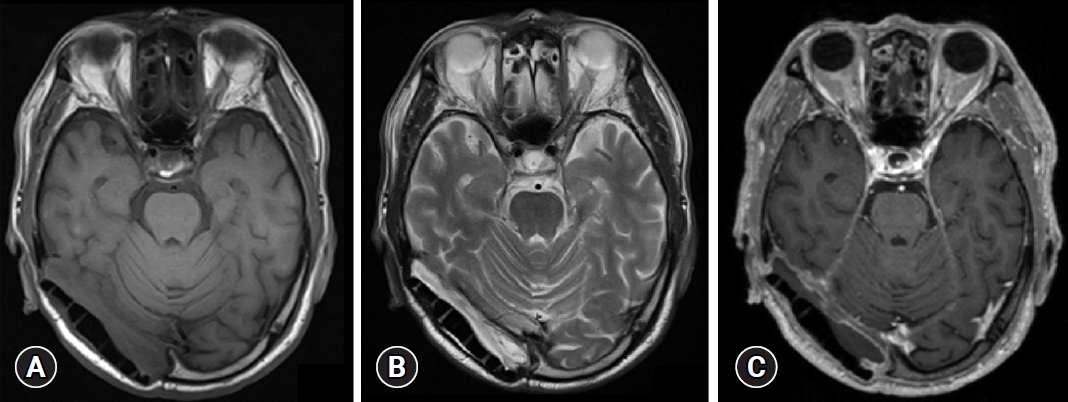
The patient was followed-up at an outpatient clinic, and no remnant tumor observed on follow-up MRI at 8-month (Fig. 4). Despite the lack of significant differences in overall cortical functions, such as memory and cognitive ability, but spatial recognition and motor coordination improved after surgery. In addition, the patient could perform some activities of daily life independently and without gait disturbance. Improvement was confirmed on follow-up examination, with an mRs: 2, and a K-MMSE score: 17/30.
IECs can occur anywhere in the skull and at any time during lifetime, but usually appear around the 4th decade [4,5]. As the tumor gradually proliferates, it compresses the surrounding parenchymal and vascular structures, leading to the appearance of symptoms [6].
Post-traumatic calcified epidermoid cysts are rarely reported [7]. We hypothesized that after head trauma with deep laceration and bone contusion some epidermal cells invased in the intracranial space and slowly developed into an IEC over a long time. As the occipital lobe acts as a center of processing, integration, and interpretation of visual stimuli [8], these functions can deteriorate due to the mass effect of the tumor compressing this area found in our case. As reported here, surgical treatment can be helpful for improving the neurological deficits by decreasing the mass effect [9]. Complete resection, which sometimes includes dura mater removal and repair, is important to prevent progression and bone erosion, and to reduce the risk of infection and aseptic meningitis [10]. However, if the capsule strongly adheres to the surrounding neurovascular structure, it is better to avoid complete removal and perform a conservative surgery instead [11].
The results of this case suggest that resection of an epidermoid cyst with parenchymal compression would help improve cortical function. However, it is only a result of one case, and it is difficult to derive statistically significant results, so it is thought that research through many cases is necessary.
Fig.┬Ā1.
Preoperative magnetic resonance imaging (MRI) findings. (A) T1, (B) T2, and (C) enhanced MRI. A large lobulated extra-axial tumor was observed in the right occipital convexity, with an isointense to hyperintense signal on T2 and an isointense to hypointense signal on T1. Adjacent dural thickening, direct invasion of the bone tissue, and bone destruction were observed. Inner calcification and peripheral cerebrospinal fluid cleft findings were visible, and the midline had shifted to the left due to the mass effect.
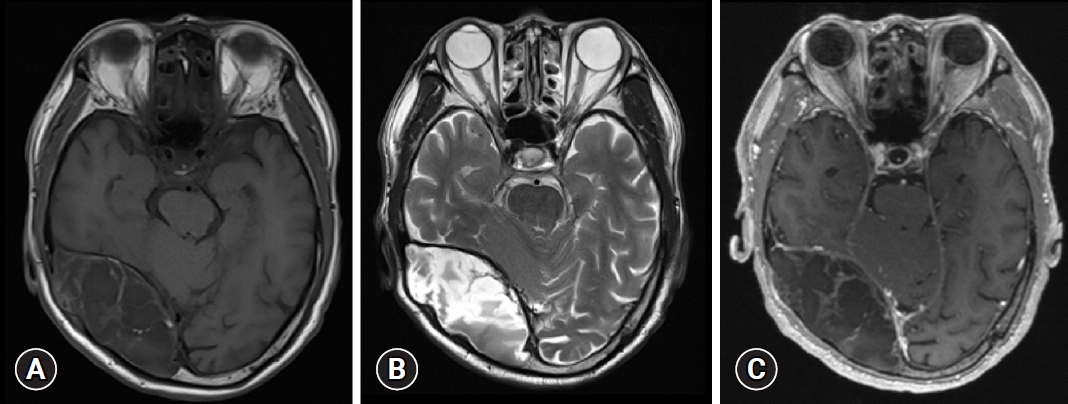
Fig.┬Ā2.
Preoperative computed tomography (CT) findings. (A) Axial view, (B) sagittal view, and (C) enhanced CT. (A, B) Note the large mass in the right occipital convexity, which was most likely the original bone mass. Fluid density was mainly visible, and soft tissue density was partially visible. (C) There were no obvious findings of enhancement.
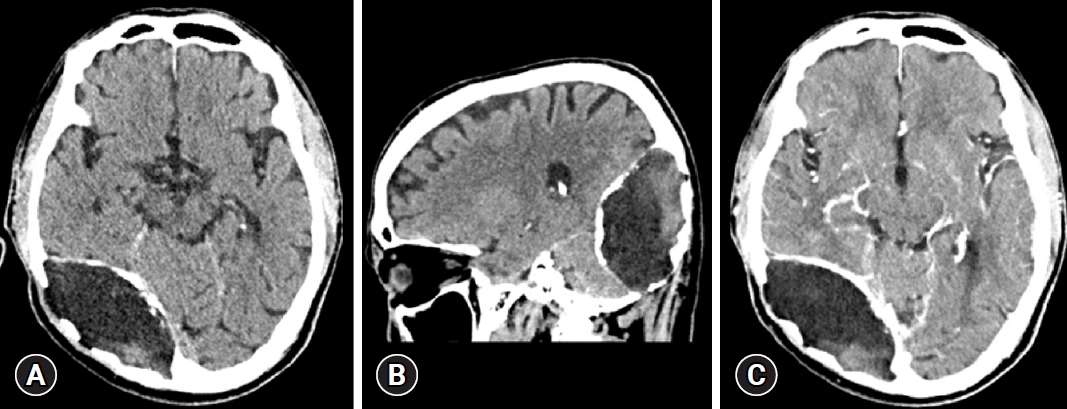
Fig.┬Ā3.
Biopsy findings. The margin was lined with stratified squamous epithelium, along with visible epithelial cell and keratin debris. No other skin adnexa was observed (H&E, ├Ś100).
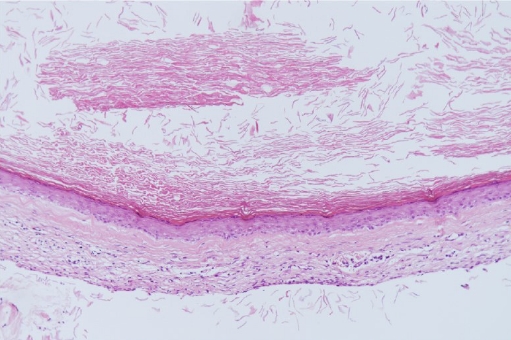
Fig.┬Ā4.
Follow-up magnetic resonance imaging (MRI) findings. (A) T1, (B) T2, and (C) enhanced MRI. No definite evidence of a remnant tumor was noted. A small amount of extra-axial fluid collection and epidural fluid collection was observed at the tumor resection site, and the mass effect had resolved compared to the previous MRI.
REFERENCES
1. Dupre DA, Pu C, Yu A, Tomycz N. Traumatic intradiploic epidermoid cyst manifest as scalp papule. BMJ Case Rep 2015;2015:bcr2014207968.doi: 10.1136/bcr-2014-207968



2. Praveen KS, Devi BI. Calcified epidermoid cyst of the anterior interhemispheric fissure. Br J Neurosurg 2009;23:90-1


3. Arana E, Latorre FF, Revert A, Menor F, Riesgo P, Lia├▒o F, et al. Intradiploic epidermoid cysts. Neuroradiology 1996;38:306-11


4. Skandalakis JE, Godwin JT, Mabon RF. Epidermoid cyst of the skull; report of four cases and review of the literature. Surgery 1958;43:990-1001

5. Garg N, Sampath S, Yasha TC, Chandramouli BA, Devi BI, Kovoor JM. Is total excision of spinal neurenteric cysts possible? Br J Neurosurg 2008;22:241-51


6. Salazar J, Vaquero J, Saucedo G, Bravo G. Posterior fossa epidermoid cysts. Acta Neurochir (Wien) 1987;85:34-9


7. Enchev Y, Kamenov B, William A, Karakostov V. Posttraumatic giant extradural intradiploic epidermoid cysts of posterior cranial fossa : case report and review of the literature. J Korean Neurosurg Soc 2011;49:53-7



8. Serences JT, Yantis S. Spatially selective representations of voluntary and stimulus-driven attentional priority in human occipital, parietal, and frontal cortex. Cereb Cortex 2007;17:284-93


9. Bikmaz K, Cosar M, Bek S, Gokduman CA, Arslan M, Iplikcioglu AC. Intradiploic epidermoid cysts of the skull: a report of four cases. Clin Neurol Neurosurg 2005;107:262-7


-
METRICS

-
- 0 Crossref
- 0 Scopus
- 3,186 View
- 18 Download
- ORCID iDs
-
Il Young Shin

https://orcid.org/0000-0001-7293-5727 - Related articles

 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



