 |
 |
| Neurofunction > Volume 20(1); 2024 > Article |
|
Abstract
Pituitary adenoma (PA) is a benign tumor that arises from the anterior pituitary gland. PA is categorized into non-functioning and functional types, and each type requires specific treatment strategies. While transsphenoidal surgery (TSS) remains the first choice of PA management, its limitations necessitate adjunctive therapies such as stereotactic radiosurgery (SRS), particularly in cases of residual or recurrent tumors. In this review, we explore the role of SRS in PA, particularly emphasizing its complementary nature with TSS treatment. Additionally, predictive factors and therapeutic considerations in SRS, including tumor volume and hormonal remission criteria, are discussed in relation to various types of functional PAs. Although SRS offers promising outcomes, it is crucial to address potential adverse effects such as hypopituitarism and visual complications, particularly in cases of radiation-induced necrosis and internal carotid artery injuries. Treatment planning strategies to avoid adverse effects are highlighted to achieve optimal therapeutic outcomes.
Pituitary adenomas (PAs) are benign tumors originating from anterior pituitary gland. These tumors are reported to account for approximately 10-17% of all primary intracranial tumors. These tumors can be classified into two main categories: non-functioning pituitary adenoma (NFPA) and functional/secretory PA. Each type presents distinct clinical features and requires specific treatment approaches. The treatment goal of NFPA is successful tumor resection. For secretory PA, normalization of abnormal hormone levels is also important. So, to confirm treatment success of PA, tumor control rate and biological remission rate are commonly used in assessing treatment outcomes.
Transsphenoidal surgery (TSS) is regarded as the gold standard for surgical resection of PA, the gross tumor resection rate varies widely depending on factors such as tumor size, location, and degree of invasion. This is because there are critical neurovascular structures surrounding the pituitary gland such as the optic pathway, optic chiasm, cavernous sinus, and internal carotid artery (ICA), which necessitate careful consideration during treatment planning. Tumor invasion into surrounding structure is frequent in PA, limiting total resection via surgical approaches. Consequently, stereotactic radiosurgery (SRS) has been commonly chosen as postoperative and adjuvant treatment.
SRS plays a pivotal role in the comprehensive management of PA, encompassing both non-functioning and functioning adenomas. While TSS stands as the first choice of PA treatment, its limitations underscore the necessity for adjunctive therapies. Consequently, adjuvant measures such as SRS assume significance in addressing residual or recurrent PA.
Unlike standalone interventions, SRS complements existing treatments, with a dual focus on achieving biochemical remission and tumor control. The notable responsiveness of PA to SRS is attributed to their hyper-water content, reinforcing its therapeutic relevance. The evolving treatment paradigm, characterized by the integration of SRS, underscores a symbiotic relationship with TSS, striving towards optimal therapeutic outcomes.
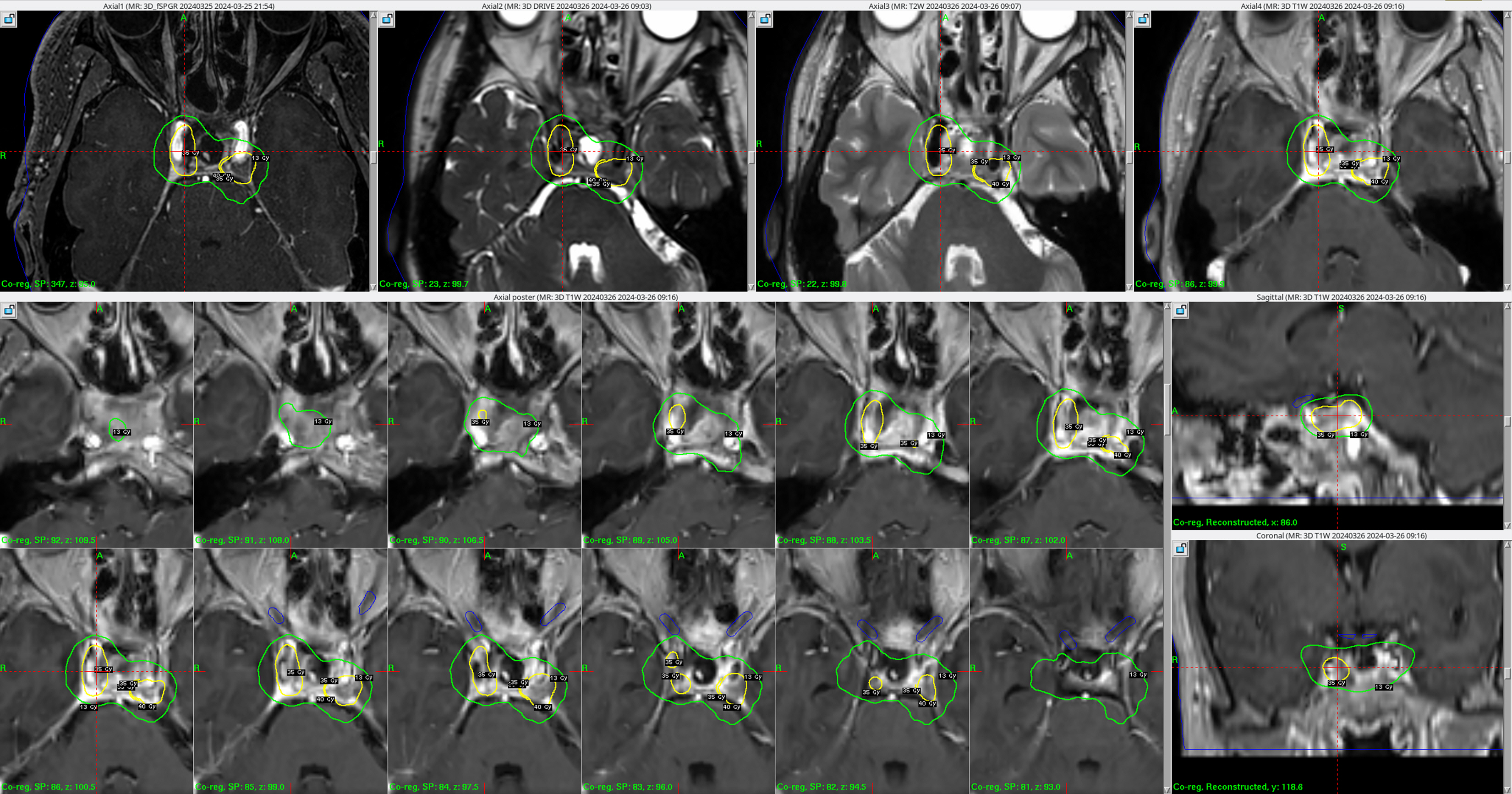
A majority of patient of NFPA have planned margin dose of 14-15 Gy in single fraction SRS [1] and the dose to the optic nerve pathway is the most important factor in determining the margin dose. In case of secretory PA, margin dose have selected 20-30 Gy. Higher margin dose is known to increase the success rate of hormonal normalization, but it should be set with consideration of the side effects that can occur due to high margin dose. To mitigate treatment-induced toxicity, such as optic problems, hypofractioned SRS have been considered (Fig. 1).
Hypofractionated SRS dose is planned as 12 Gy in three fractions to 25 Gy in five fractions, equivalent to single fraction dose of 11-13 Gy [2,3]. Hypofractionated SRS has shown comparable effectiveness in tumor control rates to single fraction SRS while being safer in terms of treatment-induced toxicity, making it preferable when the risk of adverse effects on the optic apparatus is high [4].
While tumor size is often a concern in other cancers, for PAs, the key factor is functionality. So, imaging tests that can distinguish between them are essential. Surgeons have to distinguish delicate pituitary lesion of PA from surrounding normal structures. Advancements in magnetic resonance imaging (MRI) sequences, notably fast spoiled gradient recalled echo (fSPGR), play a crucial role in detecting PAs. fSPGR offers superior sensitivity compared to conventional MRI sequences, enabling visualization of both the adenoma itself and surrounding normal pituitary anatomy. This detailed visualization facilitates accurate diagnosis and treatment planning [5].
Furthermore, fSPGR imaging proves valuable in cases following TSS. In these postoperative scenarios, fSPGR provide indispensable insights for accurate detection of any residual tumor or recurrent lesions and differentiation the PA, as well as surrounding normal structures. This precise delineation is critical to SRS in adjuvant therapy.
Several key factors, including tumor volume, suprasellar extension, and marginal dose, dictate therapeutic outcomes in SRS for PA. Addressing challenges such as out-field recurrence necessitates comprehensive monitoring and management strategies. Specially, in case of secretory PA, the spectrum of hormonal remission in conditions like acromegaly and CushingŌĆÖs syndrome underscores the need for tailored treatment approaches. Secretory PAs are commonly associated with hormonal hypersecretion syndromes, with tumors secreting prolactin (PRL), growth hormone (GH), or adrenocorticotrophic hormone (ACTH) being the most prevalent. There is the outcomes of SRS in the treatment of NFPA and functional/secretory PA: acromegaly, CushingŌĆÖs disease, and prolactinomas.
Studies conducted investigation into the parameters of Gamma Knife radiosurgery (GKS) in their research. They found that tumor volume played a significant role in predicting tumor progression after GKS, especially when comparing patients with lesions smaller than 5 cm3 to smaller to those with larger lesions exceeding 5 cm3. Moreover, their research identified patients with suprasellar extension as being at heightened risk of tumor progression. In terms of treatment dosage, interestingly, marginal doses smaller than 12 Gy had an impact on tumor progression [1].
Acromegaly, a condition marked by excessive secretion GH, is primarily characterized by persistent GH hypersecretion. Many articles reported that while SRS led to tumor control rates ranging from 94% to 100%, the rates of endocrine remission varied widely, from 14% to 74%, and the time to normalization of hormone levels has been reported to vary from 2 to 5 years [6-10]. Several factors contribute to this variability, including GH and insulin-like growth factor (IGF-1) levels, tumor invasion, and margin dose influencing outcome especially depending on how the definition of endocrine remission is defined. Several consensus statements have been proposed to resolve this ambiguity. The Cortina consensus established criteria for defining remission in acromegaly, stipulating that remission occurs when a patientŌĆÖs random GH level is less than 1 ng/mL or the nadir GH level after an oral glucose tolerance test (OGTT) is less than 0.4 ng/mL, accompanied by the normalization of age- and sex-adjusted IGF-1 levels [11]. In a more recent acromegaly consensus conference, the requirement for a random GH level was omitted, retaining only the criteria of achieving a nadir GH level after OGTT less than 0.4 ng/mL and normalization of IGF-1 levels adjusted for age and sex [12].
Many studies documented the efficacy of SRS in the management of CushingŌĆÖs disease, revealing tumor control rates ranging from 83% to 100% and endocrine remission rates between 6% and 81%, and the normalization of hormone levels generally takes about 20 to 22 months [13-19]. Akin to the case of acromegaly, itŌĆÖs crucial to note the variable approach taken by researchers in defining endocrine remission across these studies. The parameters used to define endocrine remission varied among these studies, with normalization of 24 hours urinary free cortisol being a prevalent criterion [14]. Alternatively, some authors employed serum cortisol or ACTH levels, either independently or in combination with urinary levels [15,16].
In the management of prolactinomas, dopamine agonists (DAs) stand as the cornerstone of treatment due to effectiveness. However, in cases where patients exhibit resistance to DA, TSS become necessary. Additionally, SRS is employed following TSS in instances of tumor recurrence or residual growth. Studies have showed tumor control rates between 86% and 100%. Endocrine remission rates have shown considerable variability, spanning from 5% to 50%, and generally, it takes around 14 and 20 months for PRL levels to normalize post-treatment [20-23], with criteria for defining remission varying across studies. This is likely due to the fact that the level of PRL after treatment varies between institutions and suggests that further discussion is needed.
SRS stands as a valuable tool in the management of PAs, yet it is imperative to acknowledge and mitigate potential adverse effects associated with this treatment modality.
One significant complication following SRS for PA is delayed hypopituitarism. This endocrine disorder arises from damage to the surrounding healthy pituitary gland or stalk, which are located in close proximity to the PA. Studies report an incidence of hypopituitarism as high as 24.5% following GKS for NFPA after TSS, and to reduce this, radiation dose to the infundibulum is proposed to be a mean dose of 7.56 Gy and a maximum dose of 12.3 Gy [24]. This underscores the critical role of meticulous dosage planning and treatment strategy in minimizing the risk of this adverse effect. Precise targeting that minimizes radiation exposure to the healthy pituitary gland and stalk is crucial. Careful consideration of treatment protocols, including dose fractionation and margins, is essential for effective management and reducing the incidence of delayed hypopituitarism.
While SRS offers a safe and noninvasive treatment for PA, visual complications remain a potential concern. The reported incidence of visual disturbances following SRS is fortunately low, typically less than 1%. However, meticulous treatment planning is essential to minimize this risk. Stringent dose limitations are applied to the optic pathway to safeguard against radiation-induced neuropathy. The maximum tolerated dose to the optic chiasm and optic nerves is generally considered to be 8-10 Gy [25]. Treatment planning software meticulously calculated the radiation distribution to ensure these critical structures remain below this threshold. Additionally, maintaining a safe distance between the tumor margin and optic apparatus is another crucial strategy to mitigate visual complications. Ideally, 1-5 mm should be maintained between the tumor and the optic structures [26]. This buffer zone helps to minimize the radiation dose delivered to the optic nerve. However, in certain cases with anatomical limitations or complex tumor shapes, maintain this ideal distance may not be feasible. Advanced SRS techniques using GKS, such as dynamic shaping (Perfexion®) and hypofractionated GKS (ICON®), offer promising solutions for these challenging scenarios. Hypofractionated SRS involves delivering the prescribed dose in fewer, larger fractions, potentially reducing the overall risk of complications compared to conventional fractionation schemes.
In cases where radiation induced necrosis develops, particularly in invasive PA, necrosis can potentially lead to cranial neuropathies. This risk is heightened due to the close proximity of PA to critical structures such as the ICA, cavernous sinus and brain stem. In case of brain stem, the exposure is designed to be less than 15 Gy [27]. Also, minimizing the risk of vascular injury is crucial in SRS for PA. Irradiation of suprasellar extension can cause irradiation of the circle of Willis, and irradiation effect of the ICA should be considered for covering parasellar extension [28]. Irradiation to each artery promotes atherosclerosis, which increases the risk of cerebrovascular accident and stroke. One approach to prevent this is by limiting the radiation coverage to ensure it does not exceed more than 50% of the vessel diameter [29]. Additionally, exceeding a dose of 30 Gy to the ICA should be avoided. Exposure to such high radiation doses can induce a neo-intimal hyperplasia response in smooth muscle cells lining the vessel, potentially leading to vascular injury. While the risk is relatively low, studies have reported that exposure to radiation doses ranging from 15 to 25 Gy may increase the risk of post-radiosurgical stenosis or occlusion in approximately 1% of patients [30]. This highlights the importance of treatment planning to minimize ICA exposure whenever possible.
PAs present a complex therapeutic challenge, requiring a multidisciplinary approach for effective management. While TSS remains the primary treatment modality, SRS assumes a crucial role, particularly in cases of residual or recurrent tumors. The integration of SRS with advanced imaging modalities, such as fSPGR MRI sequences, enhances treatment precision and facilitates accurate diagnosis and postoperative monitoring. However, the efficacy of SRS must be balanced against potential adverse effects, including hypopituitarism and visual complications, necessitating meticulous treatment planning to minimize risks. Strategies to mitigate vascular injury, such as limiting radiation coverage and adhering to dose thresholds for the ICA, are essential for optimizing therapeutic outcomes. Moving forward, further research into predictive factors and refined treatment protocols will continue to enhance the role of SRS in the comprehensive management of PAs, ultimately improving patient outcomes and quality of life.
Fig.┬Ā1.
Hypofractionated GKS for acromegaly. A patient who underwent TSS after the diagnosis of acromegaly received hypofractionated GKS in three fractions for a residual adenoma in the left cavernous sinus and another lesion. To ensure precise identification of the target lesions, fSPGR sequences were utilized. Simultaneously, while the radiation dose was set for the target lesion, the predicted irradiation dose to the optic apparatus (shown in blue in the figure) was measured in order to protect it, and it was controlled at 10 Gy. GKS: Gamma Knife radiosurgery, TSS: transsphenoidal surgery, fSPGR: fast spoiled gradient recalled echo.
REFERENCES
1. Sheehan JP, Starke RM, Mathieu D, Young B, Sneed PK, Chiang VL, et al. Gamma Knife radiosurgery for the management of nonfunctioning pituitary adenomas: a multicenter study. J Neurosurg 2013;119:446-56


2. Liao HI, Wang CC, Wei KC, Chang CN, Hsu YH, Lee ST, et al. Fractionated stereotactic radiosurgery using the Novalis system for the management of pituitary adenomas close to the optic apparatus. J Clin Neurosci 2014;21:111-5


3. Iwata H, Sato K, Tatewaki K, Yokota N, Inoue M, Baba Y, et al. Hypofractionated stereotactic radiotherapy with CyberKnife for nonfunctioning pituitary adenoma: high local control with low toxicity. Neuro Oncol 2011;13:916-22



4. McTyre E, Helis CA, Farris M, Wilkins L, Sloan D, Hinson WH, et al. Emerging indications for fractionated Gamma Knife radiosurgery. Neurosurgery 2017;80:210-6




5. Patronas N, Bulakbasi N, Stratakis CA, Lafferty A, Oldfield EH, Doppman J, et al. Spoiled gradient recalled acquisition in the steady state technique is superior to conventional postcontrast spin echo technique for magnetic resonance imaging detection of adrenocorticotropin-secreting pituitary tumors. J Clin Endocrinol Metab 2003;88:1565-9


6. Attanasio R, Epaminonda P, Motti E, Giugni E, Ventrella L, Cozzi R, et al. Gamma-knife radiosurgery in acromegaly: a 4-year follow-up study. J Clin Endocrinol Metab 2003;88:3105-12


7. Sala E, Moore JM, Amorin A, Martinez H Jr, Bhowmik AC, Lamsam L, et al. CyberKnife robotic radiosurgery in the multimodal management of acromegaly patients with invasive macroadenoma: a single centerŌĆÖs experience. J Neurooncol 2018;138:291-8



8. Kim EH, Oh MC, Chang JH, Moon JH, Ku CR, Chang WS, et al. Postoperative Gamma Knife radiosurgery for cavernous sinus-invading growth hormone-secreting pituitary adenomas. World Neurosurg 2018;110:e534-45


9. Iwata H, Sato K, Nomura R, Tabei Y, Suzuki I, Yokota N, et al. Long-term results of hypofractionated stereotactic radiotherapy with CyberKnife for growth hormone-secreting pituitary adenoma: evaluation by the Cortina consensus. J Neurooncol 2016;128:267-75



10. Lee CC, Vance ML, Lopes MB, Xu Z, Chen CJ, Sheehan J. Stereotactic radiosurgery for acromegaly: outcomes by adenoma subtype. Pituitary 2015;18:326-34



11. Giustina A, Chanson P, Bronstein MD, Klibanski A, Lamberts S, Casanueva FF, et al. A consensus on criteria for cure of acromegaly. J Clin Endocrinol Metab 2010;95:3141-8


12. Melmed S, Bronstein MD, Chanson P, Klibanski A, Casanueva FF, Wass JAH, et al. A Consensus Statement on acromegaly therapeutic outcomes. Nat Rev Endocrinol 2018;14:552-61




13. Bunevicius A, Sheehan D, Lee Vance M, Schlesinger D, Sheehan JP. Outcomes of CushingŌĆÖs disease following Gamma Knife radiosurgery: effect of a centerŌĆÖs growing experience and era of treatment. J Neurosurg 2020;134:547-54


14. Grant RA, Whicker M, Lleva R, Knisely JP, Inzucchi SE, Chiang VL. Efficacy and safety of higher dose stereotactic radiosurgery for functional pituitary adenomas: a preliminary report. World Neurosurg 2014;82:195-201

15. Marek J, Je┼Škov├Ī J, H├Īna V, Kr┼Īek M, Li┼Ī─Ź├Īk R, Vladyka V, et al. Gamma knife radiosurgery for CushingŌĆÖs disease and NelsonŌĆÖs syndrome. Pituitary 2015;18:376-84


16. Narayan V, Mohammed N, Bir SC, Savardekar AR, Patra DP, Bollam P, et al. Long-term outcome of nonfunctioning and hormonal active pituitary adenoma after Gamma Knife radiosurgery. World Neurosurg 2018;114:e824-32

17. Sheehan JP, Xu Z, Salvetti DJ, Schmitt PJ, Vance ML. Results of gamma knife surgery for CushingŌĆÖs disease. J Neurosurg 2013;119:1486-92


18. Wein L, Dally M, Bach LA. Stereotactic radiosurgery for treatment of Cushing disease: an Australian experience. Intern Med J 2012;42:1153-6

19. Wilson PJ, Williams JR, Smee RI. CushingŌĆÖs disease: a single centreŌĆÖs experience using the linear accelerator (LINAC) for stereotactic radiosurgery and fractionated stereotactic radiotherapy. J Clin Neurosci 2014;21:100-6

20. Cohen-Inbar O, Xu Z, Schlesinger D, Vance ML, Sheehan JP. Gamma Knife radiosurgery for medically and surgically refractory prolactinomas: long-term results. Pituitary 2015;18:820-30



21. Liu X, Kano H, Kondziolka D, Park KJ, Iyer A, Shin S, et al. Gamma knife stereotactic radiosurgery for drug resistant or intolerant invasive prolactinomas. Pituitary 2013;16:68-75



22. Tanaka S, Link MJ, Brown PD, Stafford SL, Young WF Jr, Pollock BE. Gamma knife radiosurgery for patients with prolactin-secreting pituitary adenomas. World Neurosurg 2010;74:147-52


23. Wilson PJ, Williams JR, Smee RI. Single-centre experience of stereotactic radiosurgery and fractionated stereotactic radiotherapy for prolactinomas with the linear accelerator. J Med Imaging Radiat Oncol 2015;59:371-8


24. Oh JW, Sung KS, Moon JH, Kim EH, Chang WS, Jung HH, et al. Hypopituitarism after Gamma Knife surgery for postoperative nonfunctioning pituitary adenoma. J Neurosurg 2018;129:47-54


25. Leavitt JA, Stafford SL, Link MJ, Pollock BE. Long-term evaluation of radiation-induced optic neuropathy after single-fraction stereotactic radiosurgery. Int J Radiat Oncol Biol Phys 2013;87:524-7


26. Kamogawa M, Shuto T, Matsunaga S. Effects of two different radiotherapies for craniopharyngiomas using stereotactic radiosurgery/ stereotactic radiotherapy or fractionated stereotactic radiotherapy. Surg Neurol Int 2022;13:563



27. Mayo C, Yorke E, Merchant TE. Radiation associated brainstem injury. Int J Radiat Oncol Biol Phys 2010;76:S36-41



28. Ito H, Onodera H, Sase T, Uchida M, Morishima H, Oshio K, et al. Percutaneous transluminal angioplasty in a patient with internal carotid artery stenosis following gamma knife radiosurgery for recurrent pituitary adenoma. Surg Neurol Int 2015;6:S279-83



-
METRICS

-
- 0 Crossref
- 0 Scopus
- 50 View
- 2 Download
- ORCID iDs
-
Jung Woo Yu

https://orcid.org/0009-0001-2682-1937Won Seok Chang

https://orcid.org/0000-0003-3145-4016 - Related articles
-
Stereotactic radiosurgery for brain metastases2024 June;20(1)
Stereotactic radiosurgery for dural arteriovenous fistula2021 September;17(2)
The mixed era of stereotactic radiosurgery and radiotherapy2021 June;17(1)

 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



